RETINAL DISEASES
Diabetic Retinopathy
If you have diabetes and are experiencing changes in your vision, you may have diabetic retinopathy. At Eye Associates, our Retina Specialist, Dr. Kurt Jackson has the expertise required to provide you with the quality care needed to protect the health of your eyes and vision.
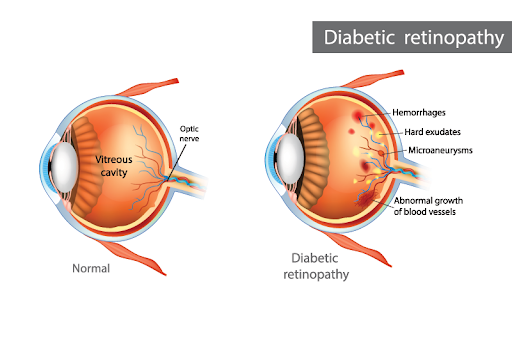
What is Diabetic Retinopathy?
Diabetic retinopathy is an eye condition that is caused by diabetes. Like other parts of your body, diabetes can cause damage to your eyes. To avoid vision damage from untreated diabetic retinopathy, it’s best to see your eye doctor for regular exams. This eye condition often occurs when blood sugars are not controlled for a period of time. When your blood sugars are high, it can cause damage to the blood vessels at the back of your eye. When these blood vessels are damaged, they can begin to swell and leak, significantly impacting your vision. Consistently high blood sugar can also cause abnormal blood vessels to grow. When either of these situations occurs, it can affect your vision.
How Do Eye Doctors Test for Diabetic Retinopathy?
If you have diabetes, your primary care provider will likely recommend that you are seen by your eye doctor at least once a year. The purpose of these exams is to ensure that there have not been any changes in your vision or your eyes due to diabetes.
At your yearly diabetic eye exam, your eye doctor will ask a variety of questions about your general health and your vision. In addition, your eye doctor will likely ask you about your A1C and current blood sugar levels. These levels will give your eye doctor information about how well controlled your diabetes is. Your eye doctor will also want to dilate your eyes at this visit.
There are many different conditions that can occur in the back of the eye. Without dilation, there is no way to view these structures and determine if they are healthy or not. Your eye doctor will also check your vision to ensure no changes have occurred since the last visit. Once dilated, your doctor will use a special lens and a microscope to view your retina. If your eye doctor detects diabetic retinopathy, they will be able to develop a treatment plan.
What Are the Symptoms of Diabetic Retinopathy?
In the early stages of the condition, diabetic retinopathy often shows little to no symptoms, so it is especially important to see your eye doctor regularly if you have diabetes.
In more advanced stages of the condition, you may notice symptoms such as:
- Blurry vision
- Difficulty seeing in dim lighting or worsening night vision
- Change in color vision
- Missing or blank spots in your vision
- Fluctuating vision
- Floaters

If you notice any of these symptoms, it is essential to seek treatment right away as they can indicate changes to your eyes due to diabetes.
How Do Eye Doctors Treat Diabetic Retinopathy?
Depending on its severity, your eye doctor will develop a treatment plan for your diabetic retinopathy. There are various treatment methods available, and your eye doctor will determine the method that will best fit your needs.
In addition to establishing a treatment plan, your eye doctor will also suggest you work on regulating your blood sugar. Your blood sugar levels will need to be within the normal range for your vision to stabilize.
Our office recommends PRN Numaqula Vitamins to help support healthy macular function. Click here to view our PRN vitamins or call our office for more information:
Macular Degeneration
Macular degeneration is an eye condition that affects the central vision, causing it to be difficult to see well enough to perform everyday tasks in advanced stages. At Eye Associates, our experienced eye doctor can help treat macular degeneration to help preserve your vision.
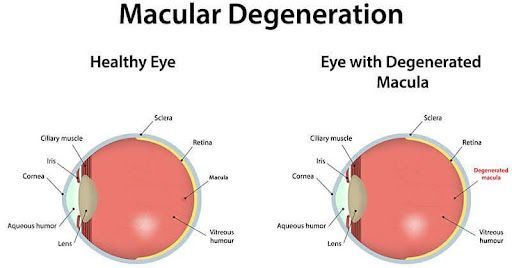
What is Macular Degeneration?
Macular degeneration is an eye condition that affects the tissue located at the back of the eye, known as the retina. This tissue is sensitive to light and transmits signals to the brain so you can see. The proper functioning of the retina is essential for crisp and clear quality vision. The macula is a location on the retina that is responsible for your central vision. Whenever you look at something directly, the macula allows you to see that image in detail. In macular degeneration, the cells responsible for central vision in the macula become damaged.
There are two types of macular degeneration: dry and wet. Dry macular degeneration often progresses gradually. There are also different stages of dry macular degeneration. Once dry macular degeneration moves from the early stage and reaches the intermediate stage, symptoms will become more apparent.
If the condition progresses and passes the late stage, it may worsen and transition into wet macular degeneration. Wet macular degeneration is the more severe type and can cause serious central vision changes that require treatment.
Although wet macular degeneration is less common, it can cause vision damage much quicker than dry macular degeneration.
What causes Macular Degeneration and who is at risk for developing it?
Macular degeneration is often also called age-related macular degeneration. This is because most people who develop macular degeneration develop the disease due to age. As you age, your macula will begin to thin over time. Due to this, age is the factor that causes you to be at the highest risk for developing macular degeneration.
Macular degeneration is characterized by the growth of abnormal blood vessels in the retina. When these blood vessels swell and leak, there is damage caused to the macula. Experts do not know the exact cause of the development of abnormal blood vessels. However, there is evidence that smoking and having a family history of the condition may make you at higher risk for developing it.
What Are the Symptoms of Macular Degeneration?
Early macular degeneration typically does not cause many symptoms. Although, if the condition progresses to the late stages or transitions to wet macular degeneration, symptoms will be more apparent.
The symptoms of macular degeneration often vary from person to person. However, some of the most common symptoms of the condition are:
- Straight lines appear crooked, wavy, or distorted
- Difficulty seeing in low-lighting
- Blurry, missing, or distorted central vision
- Colors appear dull or diluted
If you notice any of these symptoms, especially changes in central vision or if straight lines appear wavy, visit your eye doctor right away.
What it’s like to see with Macular Degeneration:

How do eye doctors treat Macular Degeneration?
There is no treatment available for macular degeneration when it is in the dry stage. If you have dry macular degeneration, your eye doctor will continue to monitor your eyes for changes in the condition.
Your eye doctor will likely want to see you regularly to ensure that the condition is not worsening or progressing to wet macular degeneration. They may also recommend that you begin taking special vitamins that can prevent or slow the condition’s progression.
Wet macular degeneration, although more severe, is treatable. Our Retina Specialist at Eye Associates performs Anti-VEGF injections to treat wet macular degeneration.
These injections aim to prevent vision loss by preventing new growth of abnormal blood vessels and current abnormal blood vessels from leaking.
Our office recommends PRN Numaqula Vitamins to help support healthy macular function. Click here to view our PRN vitamins or call our office for more information:
(973) 366-1232
Flashes & Floaters
Although sometimes harmless, floaters and flashes of light can signify imminent vision changes, and they're worth paying attention to. At Eye Associates, our experienced doctors have the training and expertise to help prevent any vision loss and ensure your eyes are healthy for years to come.
What are Floaters?

The retina is a photosensitive layer of receptors located at the back of your eye. In front of the retina is a gel called the vitreous. The vitreous gel fills the majority of the space inside your eye. Floaters are spots in your field of vision that can appear as small specks, lines, circles, cobwebs, or smoke. Sometimes, people assume these floaters are gnats or bugs flying in front of their faces. However, floaters are spots floating inside your eye and tend to move with your eye movement. They are tiny clumps inside the vitreous gel that cast a shadow on your retina and are often more apparent when looking at a light background, such as a sheet of paper or the sky.
There are various causes for floaters, and they are very common. As you age, the vitreous gel begins to shrink. Due to this, you will likely experience floaters as you age. In some cases, floaters are harmless, and your brain will learn to ignore them over time. However, many new or large floaters can indicate a possible retinal detachment. If you notice new floaters that look like they are raining inside your eye or large cobweb floaters, schedule an appointment with your eye doctor right away.
What Are Flashes?
Flashes of light often occur when the vitreous gel tugs or pulls on the retina. Some people describe flashes as lightning bolts or shooting stars. Like with floaters, flashes can also occur during aging as the vitreous gel shrinks and changes. Seeing flashes of light infrequently may be a normal symptom of aging in your eye. However, flashes can also indicate a possible retinal detachment, especially when paired with new or large floaters. When the retina becomes detached from the back wall of the eye, it can cause permanent vision loss.
Immediate symptoms of retinal detachment are an increase in floaters and consistent flashes. In addition to these symptoms, some people report changes in peripheral vision. If it looks like someone is pulling a curtain, shade, or veil over your vision, this could signify a possible retinal detachment. If you notice any of these symptoms, it is essential to visit your eye doctor urgently to preserve your vision.
Retinal Detachment & Tears
Retinal detachment and retinal tears can cause permanent vision loss if not treated promptly. At Eye Associates, our experts are dedicated to providing exceptional care to ensure that your vision is preserved for years to come.
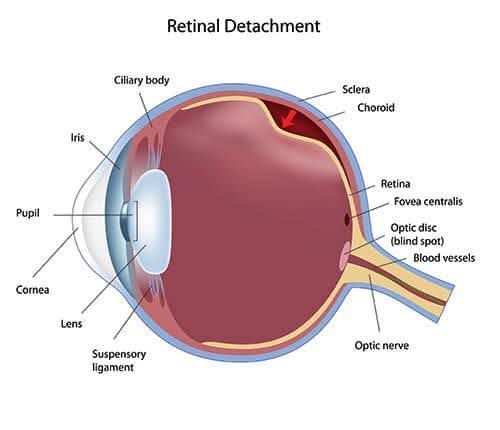
What is a Retinal Detachment?
The retina is a layer of light-sensitive tissue located in the back wall of the eye. This layer of tissue is essential for clear and crisp vision.
When a retinal detachment occurs, this tissue pulls away from the back of the eye. This can cause various symptoms, including severe vision loss.
As your eyes and body age, many changes occur. One change that happens specifically in the eye is that the gel that fills the majority of your eye called the vitreous begins to shrink. When this gel shrinks, it can tug away or separate from the retina.
This is called a posterior vitreous detachment or PVD. Sometimes, a PVD can pull on the retina and allow fluid to accumulate behind the retina and in front of the back wall of the eye. In the worst-case scenario, the retina can completely detach from the back wall in various locations. A retinal detachment often causes immediate vision symptoms and requires prompt treatment to preserve vision.
What is a Retinal Tear?
A retinal tear is when a hole or tear is created in a portion of the retina. A retinal tear can lead to a more serious retinal detachment. Similar to a retinal detachment, retinal tears often occur due to the shrinkage of the vitreous gel. Depending on the location of the retinal tear, you may experience blurry vision.
What are the symptoms of Retinal Detachment and/or Retinal Tears?
A retinal detachment and retinal tears may have similar symptoms. Although symptoms may vary from person to person, there are a few common symptoms:
- Flashing lights
- New or increased floaters
- Changes in peripheral vision or seeing what appears to be a curtain or shade coming across your vision
If you experience any of these symptoms, visit your eye doctor right away. If your symptoms are a result of a retinal tear or detachment, your eye doctor may need to begin treatment immediately.
How do eye doctors treat Retinal Detachments?
If your retinal detachment requires treatment, eye doctors have many options at hand to remediate this condition such as photocoagulation or other surgical procedures like the scleral buckle and vitrectomy.
Both photocoagulation and laser therapy procedures aim to create scar tissue to help the retina reattach to the eye wall, similar to using laser therapy to treat retinal tears. During the scleral buckle procedure, your eye doctor will place a silicone band around the eye.
This band will slightly alter the shape of your eye to help the retina re-adhere to the eye’s surface. In some cases, eye doctors perform a vitrectomy to remove all of the vitreous gel inside the eye.
How do eye doctors treat Retinal Tears?
Not all retinal tears require treatment. If your retinal tear does not require immediate treatment, your eye doctor will likely monitor your eyes to ensure that the tear is not worsening. In some cases, it may be important to treat the retinal tear to prevent a possible future retinal detachment. To do this, our Retina Specialist uses laser therapy to treat retinal tears.
Other Retinal Problems
Macular Edema
Macular edema is the swelling of the macula, which is the center part of the retina that gives us sharp reading vision. The accumulation of fluid causes visual distortion and blurred vision. There are various causes for macular edema, including diabetic retinopathy, retinal vein occlusion, uveitis (inflammation), age-related macular degeneration, and ocular surgery. This is the most common cause of vision loss in diabetics.
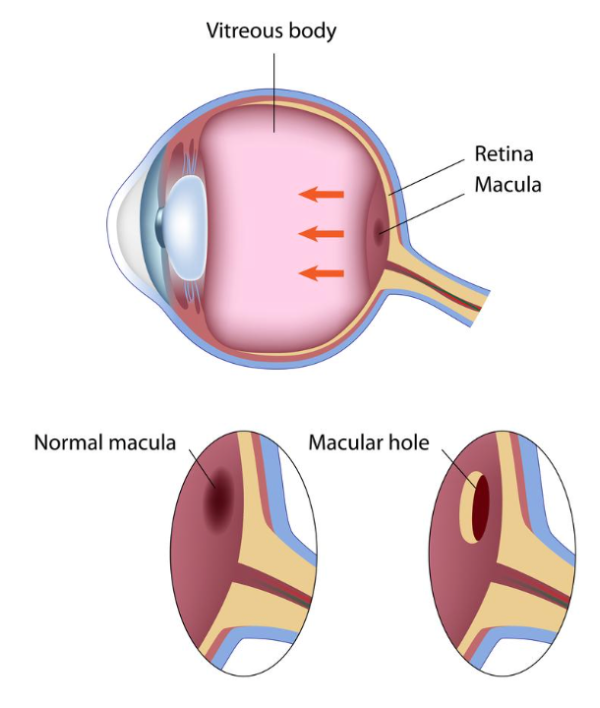
Macular Hole
A macular hole is a defect in the macula, which is the center part of the retina that gives us sharp reading vision. Macular holes usually develop as a result of the natural aging process and are known as idiopathic macular holes. These tend to occur primarily in people in their 60s to their 80s. Less commonly, macular holes can be caused by blunt trauma or seen in patients with retinal detachments or severe swelling of the retina. In the early stages of macular hole formation, the hole may only cause a small distortion of the central vision. As the macular hole progresses, the vision will worsen but will not cause complete blindness.
Macular Pucker
Epiretinal membrane (ERM) or macular pucker is the result of a semi-translucent membrane on the inner retinal surface. ERM can be idiopathic and is relatively common in patients over age 50, and both sexes are equally affected. Secondary ERM occurs regardless of age and sex due to inflammation, retinal tears/detachment, or bleeding in the vitreous.
Retinal Vein Occlusion
Retinal vein occlusion is a common vascular disorder of the retina. Obstruction of the retinal vein at the optic nerve is referred to as central retinal vein occlusion (CRVO) and obstruction at a branch of the retinal vein is referred to as a branch retinal vein occlusion (BRVO). Most retinal vein occlusions occur after the age of 50, younger patients with retinal vein occlusion may be asked to see their internist for a thorough medical evaluation.
Branch Retinal Vein Occlusion
The symptoms of a branch retinal vein occlusion depend on which venous branch is involved. Blurred vision is a common symptom that results from macular edema (swelling in the retina). If the branch retinal vein occlusion occurs at a portion of the retina away from the central vision then it may be asymptomatic.
Central Retinal Vein Occlusion
When the central retinal vein is blocked, this will result in more blood and swelling building up in the retina and also worse vision than a branch retinal vein occlusion. Blurred vision is usually due to macular edema or glaucoma from abnormal blood vessels that develop in the eye.
- Diagnosis: A dilated eye examination is usually followed by a fluorescein angiography and optical coherence tomography.
- Treatment: One of the main complications of vein occlusion is macular edema, which is swelling in the central part of the retina. Injections of anti-vascular endothelial growth factors and steroids may help treat macular edema.